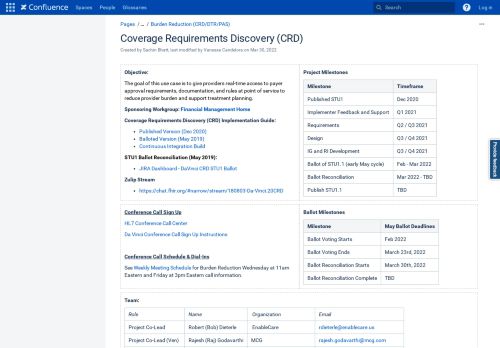
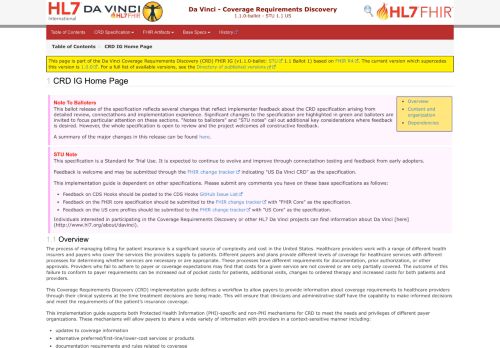
HL7 FHIR® Implementation Guide: Coverage Requirements Discovery, Release 2.0.1
Product Family
Realm
Accelerator
Specification Type
Workgroup
This specification provides a mechanism for healthcare providers to discover guidelines, pre-authorization requirements and other expectations from payor organizations related to a proposed medication, procedure or other service associated with a patient's insurance coverage. It supports both patient-specific and patient-independent information retrieval.
- Give Feedback on this Specification
- Specification Package in FHIR Registry: hl7.fhir.us.davinci-crd#2.0.1
- HL7 FHIR online validator
- Reference Implementation Software
CMS Interoperability and Prior Authorization Final Rule
- Recommended Implementation Guides
This specification is listed by the U.S. Centers for Medicare and Medicaid Services as a “supported IG”.
HL7 Project Insight ID: 1428
Specification Status
Status Date: 01/08/2024
Target Publication Date: 06/11/2022
Editions
This is a prior edition.
Project Contact
Publishing Contact
Vocabulary Contact